Professor Robert Paul (center) serves as the director of the Missouri Institute of Mental Health and leads a team of researchers using advanced neuroimaging and high-powered computational algorithms to get a better understanding of Alzheimer’s disease. Working with Paul are (from left) Andrew Belden, Lucette Cysique, Paola Garcia-Egan, Rebecca Preston-Campbell, Christina N. White and Jacob Bolzenius. (Photos by August Jennewein).
There are many symptoms that might make older adults – and those closest to them – start to worry about the early stages of Alzheimer’s disease and other age-related brain disorders.
They can include an increase in the frequency of fairly routine memory lapses, such as when persons forget why they walked into a room or where they last left their keys, wallet or sunglasses. In other cases, individuals might start repeating themselves during conversations.
No matter what trips the alarm for someone to go visit a doctor, newly diagnosed patients and their family members will end up facing some version of the same question: “What’s going to happen next?”
A precise answer remains elusive.
“Historically, our answer is that individuals with neuro-degenerative disorders will experience worse symptoms as the disease progresses,” University of Missouri–St. Louis Professor Robert Paul says. “But the rate of progression differs from one person to the next. We know, on average, that individuals will develop cognitive symptoms of sufficient severity to impair their ability to manage daily living skills like cooking, driving, managing their medication and staying on top of their bills.
“However, we cannot predict the timing of these progressive changes for each individual using traditional clinical techniques.”
Paul is one of the researchers trying to unlock those answers in just one of the projects he’s leading in his role as director of the Missouri Institute of Mental Health.
His team is taking a new approach, using advanced neuroimaging and high-powered computational algorithms to find solutions.
“Clinical scientists are trained to think mechanistically – variable Y is due to variable X,” Paul says. “But degenerative brain disorders are more likely to involve interactions among multiple variables that differ in small but meaningful ways for each individual, even though the final expression of symptoms looks similar.”
Technical advances and greater computing power make it possible to identify the combination of factors that work in tandem to increase individual risk.
The work Paul’s team is doing is well aligned with the goals of the University of Missouri System’s NextGen Precision Health Initiative, which aims to capitalize on advances in genetics, biology, big data, bioengineering and medical technologies to usher in a new era of personalized health care for Missourians and other clinical populations around the world. The initiative is manifested in the NextGen Precision Health Institute being built in Columbia, Missouri.
Evolution
Paul’s work also fits well with the historical origins of MIMH. The institute was established in 1962 as the Missouri Institute of Psychiatry on the grounds of the St. Louis State Hospital as the research and teaching arm of the Missouri Department of Mental Health.
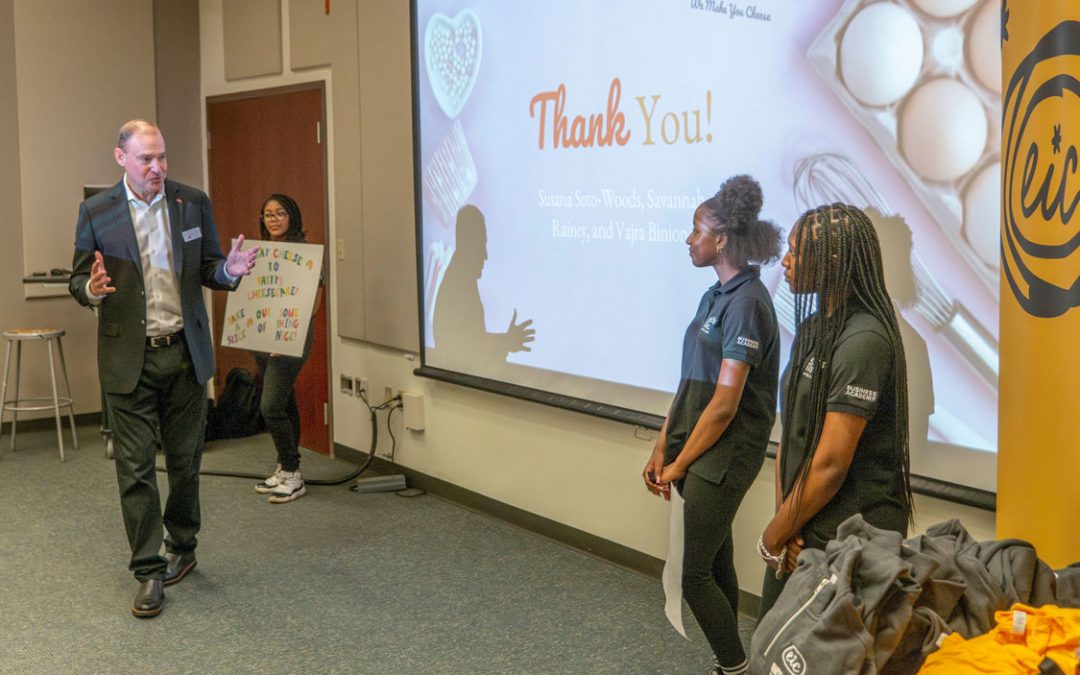
Ed Riedel brings a background in social work to his role as a project director at MIMH. He has assisted Rachel Christiansen Taube in training instructors in the Mental Health First Aid program.
The University of Missouri–Columbia School of Medicine took over its operations in 1965, though it remained in St. Louis, closely connected to the Department of Mental Health.
Much of the early work at the institute – beyond training mental health professionals for public clinical psychiatry – was in bioinformatics, the science of collecting and analyzing complex biological data, with a goal to inform patient care.
Over the years, the institute expanded its focus to include behavioral health as well as prevention, outreach and professional education and, more recently, policy research, program evaluation and public education about mental and addictive disorders.
MIMH changed its academic affiliation to UMSL as part of the Office of Research Administration in 2010, not long after Joe Parks, the chief clinical officer at the Department of Mental Health, took over as its director. Paul succeeded him in 2014, the same year the institute moved its physical location away from the state hospital to UMSL’s startup incubator, Innovative Technology Enterprises, in St. Louis County.
Each of its project teams is self-sustaining, covering expenses with grant funding. Collectively, MIMH investigators were awarded more than $9 million in external funding last year, much of it from the Substance Abuse and Mental Health Services Administration and the National Institutes of Health.
“The great thing about MIMH is that if you have a particular area of interest and you’re able to cobble together the funding, you can do it,” says Ed Riedel, a project director with a background in social work who joined the staff at MIMH in 2008. “We’ve gotten really good at writing really good grants.”
Impact
MIMH investigators cover the entire health care continuum from innovative biomarker discovery to program evaluation, professional training and community prevention, though some projects aren’t limited to a single category.
Rachel Kryah serves as the principal investigator evaluating the effectiveness of Boone County Project LAUNCH – Linking Actions for Unmet Needs in Children’s Health.
The institute manages to touch people in all 114 counties of the state. Rachel Christiansen Taube is the director of Mental Health First Aid, a public education program that teaches participants to recognize risk factors and warning signs of mental health disorders or crisis situations. Riedel also has assisted her in training all the instructors across the state – about 300 of them. Those instructors have, in turn, taken the lessons to more than 50,000 Missourians through the eight-hour training program since 2008.
“That’s one of the things I’m most proud of, and something we do really well,” Riedel says.
It is nowhere near the only thing. Senior Research Associate Brendolyn Bailey-Burch, who has been part of MIMH for more than 23 years, has worked with her team at the community level to reduce health disparities. Most recently, they’ve implemented prevention programs aimed at cutting down on substance use and the spread of HIV/AIDS and hepatitis among minorities through education.
“Our award-winning Girls Holla Back! program has reached over 1,000 African American women and girls and has had a profound impact on their lives,” Bailey-Burch says.
The program takes an intergenerational approach to substance use and HIV prevention, and it provides a platform for girls and their female caregivers to openly discuss sexual health. Bailey-Burch and her team have expanded their focus to include sexual risk avoidance education for minority youth in the St. Louis metropolitan area in an effort to reduce teen pregnancies. Riedel, Jeffrey Noel, Elizabeth Sale and Rachel Kryah all work in program evaluation, making sure that practitioners on the ground are following best practices and getting results in areas of suicide prevention, substance use disorder and children’s mental health.
Kryah has a long-standing connection with one of Columbia’s largest pediatric offices, starting with Boone County Project LAUNCH – Linking Actions for Unmet Needs in Children’s Health – evaluating the effectiveness of the social and emotional supports it provides patients through the HealthySteps program.
“We’re evaluating and working with those folks to help them measure what they’re doing and feed that back to them so that they can provide the best services possible,” Kryah says. “We have these wonderful relationships. A lot of people tend to be scared of evaluators. It feels more like we’re on the same team here. We all want the same thing.”
Rachel Winograd (third from left in the front row) directs the Missouri Department of Mental Health’s State Targeted Response and State Opioid Response projects as well as the Missouri Opioid-Heroin Overdose Prevention & Education project. She’s joined by a team of researchers at MIMH that includes (back row, from left) Alex Duello, Lillie Jackson, Sarah Phillips, Phil Horn, Aaron Ruiz, Lauren Green, Paul Thater, Sandra Mayen and Maggie Nagle and (front row, from left) Erin Stingfellow, Kori Richardson and Suzanne McCudden.
MIMH has played a substantial role in Missouri’s efforts to quell the opioid crisis that’s been surging in the state over the past decade. Associate Professor Rachel Winograd directs the Missouri Department of Mental Health’s State Targeted Response and State Opioid Response projects, launched in 2017, with the backing of two federal grants totaling over $65 million.
Winograd also leads the Missouri Opioid-Heroin Overdose Prevention & Education project, which aims to reduce overdose deaths through expanded access to overdose education and naloxone.
“What I’m excited about is how comprehensive we’re trying to make our work and our approach,” Winograd says. “We have our fingers in all types of drug and opioid-related data from all over the state and communicate with medical examiners looking at death reports to really get a sense of patterns and trends and emerging threats that are happening in Missouri from a public health and epidemiological standpoint.
“Then we have team members who are going out into the community and doing trainings or giving naloxone in barber shops or homeless shelters and actually implementing programs that work to save lives. We design clinical strategies and approaches, influence state policy and create research documents and publish papers highlighting our findings. There’s not an aspect of drug use or addiction or overdose that we’re not touching.”
As focused as many MIMH researchers are on initiatives in Missouri, the institute’s work also stretches beyond its borders and around the globe to more than 15 countries.
Paul is part of an international consortium working with long-range data from HIV/ AIDS patients in Bangkok, Thailand, exploring the dynamics between infection, the immune system’s response and the impact on the brain.
“The value of this place is the strength of all the teams,” Paul says. “UMSL leadership has fostered a research culture that allows innovation, creativity and resources to go after the most vexing challenges related to mental health, including clinical conditions others might consider impossible to resolve. For our teams, the question isn’t if we can solve the problem but rather how quickly? And we are moving very fast at present.”
This story was originally published in the fall 2019 issue of UMSL Magazine. If you have a story idea for UMSL Magazine, email magazine@umsl.edu.