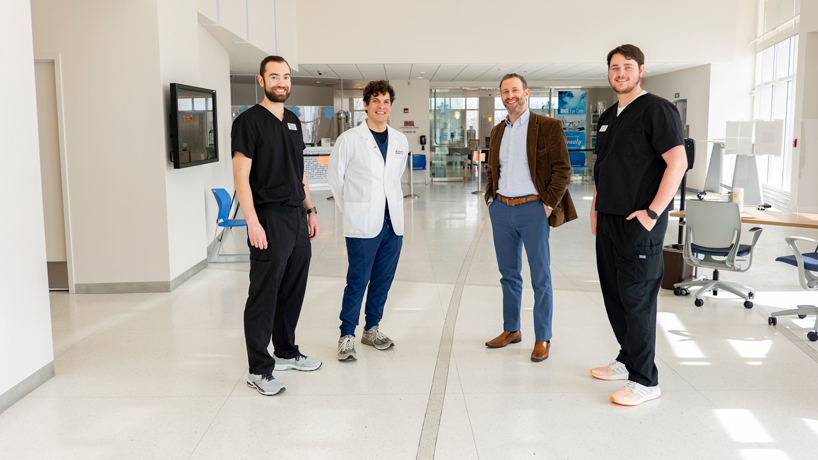
UMSL Assistant Clinical Professor of Optometry Tareq Nabhan (second from right) launched “Introduction to Telehealth” last semester. The course aims to inform third year students such as (from left) John Kingsley, Heath Rolwing and Cole Stanton on the possibilities of tele-retinal and tele-optometry services. (Photo by August Jennewein)
Until a handful of years ago, telehealth didn’t mean too much in optometry.
For many, it’s brought to mind dubious websites selling contacts or glasses without prescriptions or outdated ones, potentially endangering health for the sake of profit and convenience.
“But that’s not really telehealth,” said Tareq Nabhan, an assistant clinical professor of optometry at the University of Missouri–St. Louis. “Telehealth is truly keeping patients at the center of the experience, getting to patients using technology, in a thoughtful way.”
Advances in optometric technology have changed the scope of possibilities. Now optometrists can reach patients through advanced tele-optometry and tele-retinal services that didn’t exist even a decade ago. That’s opening doors for patients during the pandemic and those living in underserved areas of the U.S. and abroad.
Nabhan has been working to help the profession define its position on telehealth and educate the next generation of doctors. During the fall semester, he launched a new College of Optometry offering, “Introduction to Telehealth.”
The new offering helped open students’ eyes and minds to the possibilities.
“Before the class, I would say I was probably opposed to it because I want patients to come in to see me,” third-year student Heath Rolwing said. “During the class, we saw a lot of the different aspects of how telehealth can be incorporated into use and how it can be beneficial to optometry.”
The idea for the class grew from Nabhan’s long held interest in democratizing vision health care through technology. A frequent participant in overseas optometric mission trips, he’d seen how even so-called portable technology became difficult to travel with and began thinking about what could be accomplished through the advances in cellphone technology.
Shortly before the pandemic, Nabhan began putting together a proposal to teach the use of optometric telehealth at UMSL in conjunction with the federally qualified health center Affinia Healthcare, with which the college has a longtime partnership.
“With the pandemic, there was more urgency to get something like this out there that allows us to get to patients that can’t get to us, which has always been a problem pre-pandemic,” he said. “But it exposed how vulnerable systems were, not being able to deliver care during a global pandemic.”
Nabhan structured the class around visits by an impressive host of guest lecturers: Harvard University Associate Professor of Ophthalmology Jerry Cavallerano; University of Washington Assistant Professor Aaron Lee, a retina specialist and computer scientist focusing on artificial intelligence; UMSL Professor of Computer Science Sanjiv Bhatia, who lectured on the computer vision and image processing side of AI; U.S. Navy Aerospace Optometrist and Spaceflight Associated Neuro-ocular Syndrome specialist at the NASA Johnson Space Center Tyson Brunstetter; Chief Scientist, NASA Human Research Program Jennifer Fogarty, who developed the NASA telehealth program; and University of Missouri–Columbia Assistant Professor Mirna Becevic, who spoke on the implementation and ethics of telehealth systems.
They started by exploring the two types of optometric telemedicine: tele-optometry, virtual visits run through teleconferencing planforms such as Zoom; and tele-retinal services, in which photos are taken of the patient’s eyes and then later reviewed by an optometrist or ophthalmologist.
Learning about the different telehealth possibilities through the guest lectures gave the students real-life examples – none of which had a greater impression than NASA’s use of tele-retinal optometry.
“For space expeditions, they can’t just turn around and come back and be like, ‘Hey, something’s going on,’” third-year student Cole Stanton said. “They have to be able to relay information back and forth. Seeing that applied to space makes it seem like, ‘Wow, well, we can just do that on Earth, and it’d be a matter of milliseconds when I get the picture.’ It definitely opened my eyes up a lot to the technology and how our profession can move with it.”
They covered the practicalities of telehealth on Earth, as well, which runs the gamut from being incorporated into primary care visits of patients unlikely to make a separate eye health visit to creating coverage in areas without vision providers to convenience visits for patients who might not want to come or are unable to because of lack of access to transportation.
All that represents an expansion of the profession and the ability to see patients who otherwise might not have access to care.
“It’s big for diabetes,” Rolwing said. “I think less than 50% are seeing their eye doctor on the schedule they’re supposed to. So if you can catch them and get a picture while they’re at their primary care provider, you can send that on to an optometrist.”
The course also covered implementation of telehealth programs, including billing and coding as well as the Centers for Medicare & Medicaid Services’ position, and the different laws held by individual states.
With about 50 students in the course, Nabhan decided to have each one research a different state and report back to the group.
“It was definitely a pretty hard project,” said student John Kingsley, who researched Louisiana. “To find the information, you really had to dig because telehealth is such a new thing. It’s still in the new phase where people are trying to figure out what to do with it. I think COVID accelerated that.”
The College of Optometry will offer the course again in fall 2022, and Nabhan plans to keep the guest lecture structure and add a clinical component. Students will rotate in small groups through Affinia Healthcare’s tele-retinal services, which Nabhan is working on launching in the near future. He’s also the UMSL primary investigator on a Health Resources and Services Administration grant in collaboration with the University of Missouri–Columbia and the Missouri Telehealth Network aimed at finding additional ways to improve and expand on the delivery of the course and its clinical complements across community health care spaces throughout Missouri.
“It was fun to get this going,” said Nabhan, who also spoke to the American Optometric Association about the course as part of its process of developing a telehealth position statement. “I think that this is going to make us work smarter, not harder. We need to figure out what the definition of optometry will be in the future.”
As for the students in the course, they all found themselves with expanded opinions of the possibilities of telehealth.
For Rolwing, that’s meant realizing the added value it will have in his future practice, even if he prefers the face-to-face interaction with patients. Kingsley has a similar view but looks forward to seeing even more technological advances unfold. Stanton could imagine himself doing research to see the impact of telehealth in reaching patients in his hometown of Fort Smith, Arkansas.
“I think it’d be interesting to see that,” Stanton said. “It would be cool to be a part of making that happen.”