UMSL BSN student Lekia Deele conducts an A1C test during an event with Affinia Healthcare through the College of Nursing’s new Clinical-Based Education program. (Photo by Derik Holtmann)
Although the clients of Project Compassion were initially skeptical of the turkey tacos, it didn’t take long before they came back for seconds and thirds.
Just before digging in, the group at the Belleville, Illinois-based nonprofit, which offers food, clothing, toiletries, therapy and housing referrals to low-income and unhoused individuals in the community, had recently watched a cooking demonstration by a group of students in the College of Nursing at the University of Missouri–St. Louis.
The students had spent several semesters working with the clients as part of the new Community-Based Clinical Education program, designed to show students how health care is delivered in a variety of settings outside of the traditional acute care hospital experience. As they got to talking with clients over the course of the program, the students realized how many relied on fast food as a major part of their diet. For their final project in the program, they chose to demonstrate small, sustainable ways to make healthier eating choices.
“It’s greasy food, food that you know you’ll be hungry 30 minutes later,” says one of the students, Brittney Bounds, who graduated in December. “We felt like this was something that we could do to just let them know that you don’t have to be a vegetarian or completely change your diet – just make small substitutions like limiting fast food or substituting beef with turkey. We didn’t do a lot of education because we were more so connecting with them as individuals and not just teaching them. We were more so on their level and interacting with them. We ate together, and we fellowshipped. When we were done, we gave them a survey, and the results were that they are more likely to prepare food at home, and that was the goal.”
Bounds and her classmates were just a few of the nursing students who have been connecting with the community through the College of Nursing’s Community- Based Clinical Education program. In building the program, director Sheila Grigsby, an associate professor and the Dean’s Fellow for Community Engagement, sought to better integrate community health into key courses throughout the BSN program each semester. Whereas BSN students were previously only introduced to community and public health concepts in their last semester in the program, the CBCE program intentionally exposes them to nursing in community-based settings throughout their coursework.
All students in the traditional undergraduate BSN program participate in this program, which aims to provide students with unique opportunities to work with an interdisciplinary team of health care providers at various community organizations throughout St. Louis, including Affinia Healthcare, Girls Incorporated of St. Louis, PreventEd, Safe Connections and more.
“Most people spend the majority of their time outside of a hospital setting,” Grigsby says. “There are so many other things that nurses can do outside of being an acute care nurse. We’re able to expose our students to the wide variety of things that nurses can do. If they can, through this experience, understand the importance of building relationships with community organizations but more importantly with our clients, I think that we’ve achieved what we set out to do. Because that’s how you achieve wellness. That’s how you achieve community satisfaction – through being able to connect with people where they work, live and play, not when they’re in a stressful situation in the hospital. You can make a lifelong impact when you are interacting with them in their own personal settings.”
In their first clinical semester, students are introduced to volunteering and service learning through two in-person experiences. On one Saturday, they volunteer with Food Outreach, helping with food preparation and filling customer orders for the food pantry. They also present on a health topic pre-selected by the residents at Holy Angels I and II, a Cardinal Ritter Senior Services facility. Topics might include skin care and aging, maintaining a healthy weight or urinary incontinence in older adults.
In the following semesters, students are assigned to a community-based clinical agency for 20 hours each semester until their final semester. During this time, in the Community Health course, they earn 60 hours and visit the agency each week for 12 weeks. After getting to know the organization over the previous semesters, students conduct a large-scale capstone project based on the needs and requests of the agency. At the end of the semester, projects are presented to the agencies as well as the College of Nursing staff, faculty and students during the College of Nursing Research Day. While students previously developed a teaching project during the Health Promotion course, the presentations never left the classroom.
“Now the students are actually preparing something that is going to be utilized in the throughout the community gave her a better community,” Grigsby says. “It wasn’t Nursing goes far just for a class project; the projects will actually help people in the community.”
Over the program’s first few years, students have worked with many Louis, all with unique missions and needs. Students have developed projects providing education on a range of topics including healthy eating, diabetes and hypertension management, effective coping skills, maternal health, trauma-informed care and neurodivergence in the classroom.
One group worked with Community Health in Partnership Services hosting monthly blood pressure screenings and glucose screenings at a church in south St. Louis, while another developed a project on car seat safety for Cardinal Glennon Outreach. Yet another group worked with Community Women Against Hardship, providing cooking classes for residents as well as health education and resources centered on vaccinations, exercise, relaxation and diabetes.
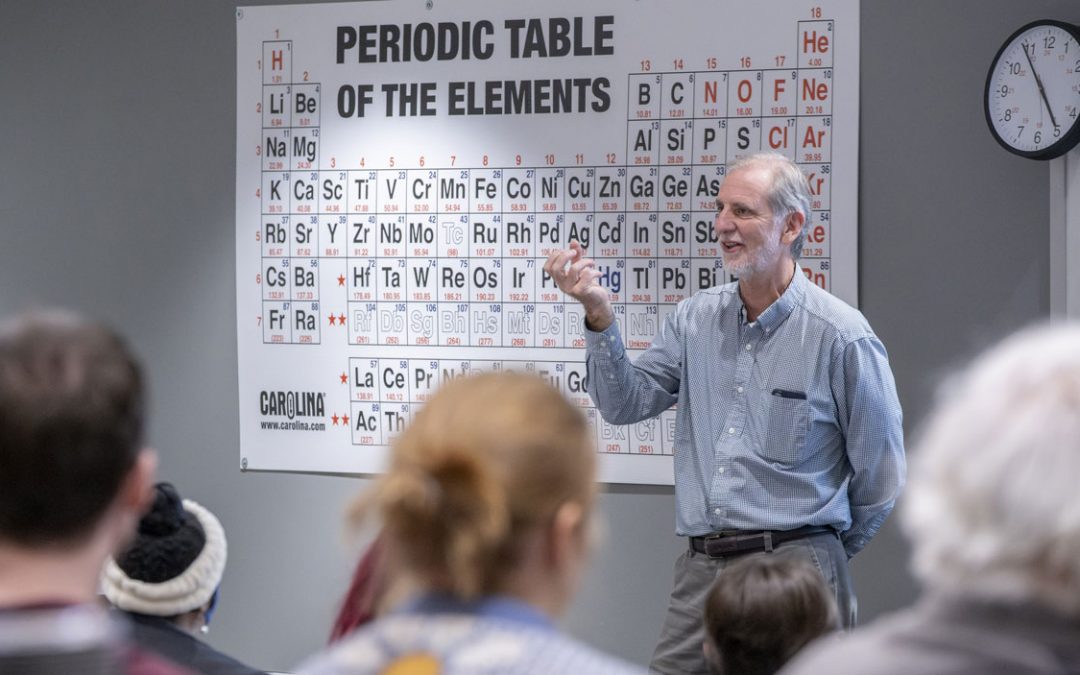
Kennady Carter, who is graduating with her BSN this spring, spent her time in the program working with Affinia Healthcare, a federally qualified health center that provides accessible and affordable comprehensive primary and preventive health care across several locations in the St. Louis area. Over several semesters working with Affinia and getting to understand patients’ needs, she assisted with HIV testing, vaccinations and sex education and also measured patients’ blood pressure in the hypertension clinic.
For their final project, Carter and her classmates studied the lack of vaccinations in children from birth to 2 years of age and the reasons parents choose not to get their children vaccinated. They found multiple factors at play, including a lack of education and pre- and postnatal care, as well as a mistrust in the health care community more broadly.
Seeing the work that Affinia does throughout the community gave her a better understanding of the way health care is delivered outside of the hospital.
“You don’t realize how many people do things differently than you do until you’re exposed to it,” Carter says. “I didn’t realize how many people used outside clinics, rather than going to a private doctor or a big hospital. Growing up, when I went to my pediatrician, I went to her office. But so many people go to this clinic where it’s basically a one-stop shop – the mom or the dad can see the dentist or the eye doctor and then the baby can see the pediatrician all in one place. It’s really nice to see that nurses are needed in these areas as well and not just in a hospital setting. A lot of times when people see nurses they think, ‘Oh, which hospital do you work at?’ But nursing goes far beyond the hospital and that’s what we’ve been able to see.”

Kennady Carter, a senior in the BSN program, discusses blood pressure results with a patient during an event with Affinia Healthcare. (Photo by Derik Holtmann)
Carter believes that understanding the different settings in which health care is delivered is key to becoming culturally competent and providing patients with an adequate level of care.
“When you go out in clinical and in the community and see what areas you’re needed in, it kind of rekindles that passion and that fire for nursing,” she says. “Having more boots on the ground in the community and helping out in that way will reduce some of those barriers to health care such as the lack of insurance, the lack of prenatal care and the lack of education. When you’re doing the work in the community, it helps educate people before they make it to the hospital and it’s an emergency.”
Students were also encouraged to get creative. December graduate Michelle Liu provided music therapy at a senior facility supported by Faith Parish Nurse Ministries by incorporating health education as she played the guitar. Lindsay Tague, also a December graduate, hosted an art therapy session in which clients of Places for People decorated Mason jars with motivational messages.
“The organizations were excited about having students work with them, but they didn’t understand the potential for how much the students could do,” Grigsby says. “I think that they appreciated the fact that they had the students there for three consecutive semesters, which really decreased the amount of training that they had to provide. The students were able to implement some very innovative programs that they had on their shelves or wish list that they wanted to do but didn’t have time to do.”
T.J. Parker, who graduated with her BSN in December, completed her clinical work with St. Andrew’s Senior Solutions with partner Maddie Malone. She enjoyed getting to know residents as she took their vital signs, tested blood pressure and glucose levels and assisted with medications and dietary questions. For her group’s final project, they taught residents to take their own blood pressure, monitor their glucose levels, make dietary changes and stay active.
Having worked in the operating room as a first assistant since 1993, Parker felt the experience allowed her to bridge the gap between what she was learning in class and put those skills to use in real life. It also offered an opportunity for her to offer a more personalized form of care, and she often returns to The Willows to visit the residents.
“Since I work in the operating room, my patients are usually asleep, so I don’t get the opportunity to see a before and after,” she says. “It allowed me to provide a level of care and then maintain relationships with clients and actually physically see the before and after. I had one client whose blood pressure was extremely high – almost stroke level. Maddie and I walked with her back to her room, and she got her daughter on the phone and went to the hospital. Something was off with her medications, and she had been on the verge of having a stroke, but I was in there and able to see what happened the next week when she was feeling better. I often don’t get to see that.”
Those are exactly the types of experiences that Grigsby and other College of Nursing clinical faculty hope to foster through the CBCE program. They’re continuing to expand and refine the program, which has seen more interest out in the community as word has begun to spread from participating agencies. When Grigsby launched the program in 2021, eight sites were on board – now, that number has grown to 30. The curriculum has also evolved and will feature three standalone courses by spring 2025.
Grigsby, who has presented the CBCE program to the Association of Community Health Nursing Educators and the American Public Health Nurse Association to positive feedback, hopes to be able to continue to share it outside of the College of Nursing. While similar nursing programs across the country offer opportunities for community health learning, many condense them into a single semester. And with 75% of UMSL graduates staying in the area after graduation, the College of Nursing’s program offers a unique opportunity for students to make an impact in their own communities.
“We’re helping our students know about the community resources that are available in the St. Louis area that can help their clients once they leave nursing school,” Grigsby says. “I think that’s a really unique aspect that we bring because we’re helping to create more well-rounded nurses once they graduate. They know about the hospital settings, but they also know about the community-based health settings as well.
“Students are more comfortable and confident to provide therapeutic conversations and communication with clients outside of a traditional health setting. They really understand social determinants of health – it’s not just a lecture. They’re actually seeing this in real life with real people. So they’re able to make the connections about what that really means and how as nurses they can make an impact with their clients.”
This story was originally published in the spring 2024 issue of UMSL Magazine. If you have a story idea for UMSL Magazine, email magazine@umsl.edu.