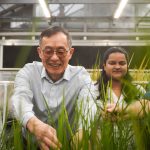
Doctor of Nursing Practice program and an associate Teaching Professor Laura Kuensting chairs the advocacy committee for the Association of Missouri Nurse Practitioners. (Photo courtesy of Laura Kuensting and graphic by Joan Barnidge)
A growing shortage of doctors around the country has many relying on advanced practice registered nurses for their primary care and other medical needs.
The core difference between an APRN and a medical doctor is in breadth of training. While a MD studies the entire lifespan, APRNs focus on one of six populations: adult geriatric, family, pediatrics, psychiatric mental health, neonatal and women’s health/gender related.
But while 23 states allow APRNs to practice to the full extent of their training – assessing, diagnosing, treating and prescribing medicine independently – the remainder place constraints that can impact population health. Missouri is one of the most restrictive states in the U.S.
But some are working to change the laws that limit practitioners. One of those advocating relentlessly is Laura Kuensting.
She’s the director of the Doctor of Nursing Practice program and an associate teaching professor in the College of Nursing at the University of Missouri–St. Louis. Kuensting has been a practicing pediatric emergency department APRN for more than 25 years and chairs the advocacy committee for the Association of Missouri Nurse Practitioners.
UMSL Daily sat down with Kuensting to talk about the challenges facing APRNs in Missouri and what she and other nurse practitioners are hoping for this legislative cycle in the latest version of the Ask an Expert series.
In Missouri how is the scope of APRN practice limited by current law?
Missouri is the most restrictive state in the nation. APRNs have to practice under a collaborative practice agreement with a physician. We’re also the one of the only states that have a mileage barrier on how far we can be away from our collaborating physician. We got that increased last year from 50 miles to 75 miles, but it’s still one of our biggest barriers.
When the tornado happened down at Joplin and wiped out Mercy Hospital in 2011, I wanted to go down and help during that crisis. I could not because it was more than 75 miles from my collaborating physician.
Is the mileage limitation literally from your office or could you go down with your collaborating physician?
I could go down with my collaborating physician if she was with me, yes. If she goes on vacation or is away for whatever reason, she has to delegate to another physician who is within that 75-mile requirement. In the rural areas, this becomes critically important because there aren’t many physicians to collaborate with, especially in the lower part of the state.
Our infant mortality rate in Missouri is one of the highest in the nation. Infant mortality rates reflect the health of the community or the health of the state or the health of the nation. Infant mortality is the death of a child up to 2 years of age. In Missouri, we’re ranked 33rd out of 50 states for infant mortality. Our maternal mortality rate is 44 out of 50 states, which means women are dying within a year after giving childbirth.
That’s because we don’t have many pediatricians or OB/GYNs in the southern, particularly the southeastern, part of the state. We only have, sparsely, family nurse practitioners. What we really need is pediatric and women’s health nurse practitioners to manage these children and pregnancies because there’s no money to attract doctors there. The practices there are really slow because there is no mass transportation that can get a patient from their house to the provider in the rural area. APRNs tend to practice in their communities, regardless of a patient’s ability to pay or the number of patient’s needed to make a practice lucrative, are more likely to make home visits, and are also more likely to accept barter as payment for services.
I have several NP colleagues who had their own practices in the rural parts of the state, but almost all of them have had to close. They were the only provider within 150 miles. They had to close down because their collaborating physician died or moved, and nobody else will collaborate with them. This is understandable because as a physician, you may become legally responsible for actions of the other provider. When you have never worked with or have limited work experience with someone, it is understandable why you may not want to collaborate with another provider. But APRNs are board certified, so the physician should have nothing to do with how APRNs treat patients.
How do APRNs make money for physicians?
If nurses own their own practices, they have to pay a collaborating physician to monitor their charts every two-to-three weeks. Commercial entities employing APRNS, such as the clinics at Walgreens and CVS pharmacies, must pay a physician to do a regular review of charts. This pay is pretty lucrative for the physician and is a bonus to their income. More importantly, the chart review does not necessarily result in a change in practice for the APRN.
Also, for example, if you’re an APRN and in a dermatology practice, you might be the provider who gives the Botox injections. On that day when you’re giving Botox, you’re generating revenue, but the whole practice gets the revenue. APRNs usually are not billing independently but instead generate an agreed-upon salary.
Medicare and Medicaid will only reimburse a nurse practitioner 85 percent of what they would pay a physician for the same services. But that’s better than nothing, so the physicians like to have us because we can extend their practices, and they’re still generating revenue from us, which is not necessarily a bad thing. The addition of at least one full-time APRN extends the capacity of the physician to treat twice the number of patients and generate revenue, and the addition of six full-time APRNs extends a physician’s capability six-fold.
Do private insurers reimburse APRNs differently?
Often times the insurance payers will not pay for NP services, so reimbursement is limited dependent on the payor. Most nurse practitioners will see patients regardless of their ability to pay, but there is a limit since APRNs must justify the expense of the practice and generate an income to support their own families. Now, the good news is CMS, the Centers for Medicaid and Medicare Services, does recognize APRNs and will reimburse us.
Why is it important for APRNs to have full scope of practice?
In Missouri, we have over 7,000 APRNs. There are over 10,000 physicians. Physicians are concentrated in the urban areas, and very few are in the rural areas where APRNs are predominant. Specialty services such as OB-GYN and psychiatry have less than 400 board-certified physicians in those areas. Board-certified APRNs can enhance services for these needs throughout the state.
Why are APRNs more likely to work in rural areas than a physician?
Because that’s where they grew up. Studies show that RNs tend to see need, and go back to school so they can come back as an APRN because they care about the health of their communities.
One of the things about our program here at UMSL is we try to actively seek practices in the rural settings to send our students for training to so they get acclimated to the difference between an urban practice and a “you’re the only health-care provider” practice.
What legislation is in the works to try to help APRNs in rural areas?
There are two upcoming bills that have to do with that 75-mile distance that APRNs can be from their collaborating physician. There’s House Bill 1816, which removes geographic proximity for all APRNs. Removing any geographic proximity for all would be a huge first step, since it really hinders women’s and psychiatric health. Then there’s House Bill 1617, regarding alternative to abortion services. This bill removes the geographic restriction for APRNs involved in providing alternatives to abortion services.
What falls under “alternatives to abortion”?
That means adopting or other family planning, such as pregnancy prevention. The Missouri legislature last year passed the law that if you’re eight weeks pregnant and or beyond, you don’t qualify for abortion services in Missouri. You’ll have to go out of state.
So HB 1617 was put forth because abortion is so restricted. Why does it make sense to waive the distance restriction for these providers?
So that we don’t get to the point where people are even considering an abortion. For those who are pregnant, we are trying to get them into resources that will not abort their baby but be able to help them manage an unwanted pregnancy and take care of the infant once the baby is born or give it up for adoption. We’re fearful that we are going to have women dying from trying to perform self-abortions. It’s critical that we’re able to get beyond that 75-mile geographic barrier, so we can get to people and talk to them about other alternatives and resources.
What do you think these bills’ chances are of passing?
This year, I think there will probably be negotiation. But our legislature is still not ready to let APRNs practice independently. There’s a lot of lobbying going on with the Missouri State Medical Association and the Missouri Association of Osteopathic Physicians and Surgeons. They have much more money than we do, and we’re a grassroots effort. They talk to those legislators every single day, and the legislators in Missouri are not willing to go against what the physicians are asking.
What about House Bill 1441 and Senate Bill 714?
In Missouri, we don’t have licenses as APRNs but only as RNs with a “document of recognition” as an APRN. These two bills are asking the legislators to let us be licensed as APRNs. The National Council of State Boards of Nursing have hired a specialist to lobby for APRN licensure in the Missouri state legislature for these two bills. While there is some speculation that the MMA and MAOPS are proposing an APRN practice bill regulated by the Board of Healing Arts, all other states have APRNs regulated by the state boards of nursing, which better fits with our training as nurses.
What would that do for APRNs?
That will help us get better reimbursement from insurance companies. The third-party payers, the private insurance companies and others argue we’re not licensed as APRNs. All other states have APRN licenses, so it’s easy to reject us as legitimate providers.
Aside from the upcoming bill, are there other changes that you would like to see happen?
Every year we have put forward a full-practice-authority bill, and it usually goes nowhere. One of my goals is to get us to a full-practice-authority state before I retire, which will be hopefully in the next five or six years. But I don’t know if that will happen. We don’t have the money for the lobbyists and the marketing and campaigning that needs to occur to be able to change a culture of physician-only care.
Are there other barriers to making that happen?
Most physicians I talk to love their nurse practitioners, but they won’t come and testify on our behalf because they’re afraid of backlash from their colleagues. We do have patients come and testify, and that is very helpful, but we need physicians to come and testify in support of what APRNs bring to the team.
For whatever reason, there’s a lot of apprehension and fear, much like when the Doctors of Optometry struggled for 50 years to get recognized as independent providers. It took about 50 years for the optometry doctorate to be recognized, and they have full practice authority now. Nurse practitioners are very much like optometrists where we can assess, treat, diagnose and prescribe, but we can’t do something like surgery. We’re not trained in it. That’s when we refer to a medical doctor such as an ophthalmologist. This is where you really need to have collaboration among the other physicians and providers who are experts in different areas, to help manage a patient.
How common is it for states to have full practice authority, which allows APRNs to evaluate and diagnose patients, prescribe medication and manage treatment?
In the U.S., we now have 23 states out of 50 that allow full practice authority. There are several more that will be turning over in the next year or two. Illinois went to full practice authority in the last year and a half. It just went into fruition this year, though. We have many APRNs going over there and opening up their own practices. That’s what happens when you’re in a restricted state, and you’re surrounded by states that have full practice authority. Because we’re so close to Illinois, I could easily go over there next week, find a building and begin my own practice. We are trying to keep Missouri APRNs in Missouri, and we are trying to strategize on how we can get people the care that they need. The most important goal for APRN practice in Missouri is to improve the health of Missourians and to use the resources we already have.